Summary
Head and neck cancers (HNCs) are the ninth most common type of cancers in the UK. Treatment can be complex and have life-changing effects that require prolonged follow-up and rehabilitative care.1 2 People living with HNC within the Thames Valley Cancer Alliance have reported long travel distances and high costs as major issues in accessing follow-up care.3 To combat this, the Care Closer to Home pilot was implemented. This provided follow-up and rehabilitative care by a multidisciplinary team at regional cancer centres. The localisation of care reduced travel times and costs, which in turn reduced fatigue and stress for people with HNCs. The pilot also reduced emergency room attendance and admission rates.2
Challenge
Head and neck cancers (HNCs) occur in approximately 20 people per 100,000 in the UK, making them the ninth most common type of cancers.1 This is up from a rate of 10.15 per 100,000 in 1990, an increase of over 100%.4 HNCs have the highest incidence rate among people aged 70–74 years, and incidence rates are over 60% higher for people in the lowest socioeconomic quintile.5
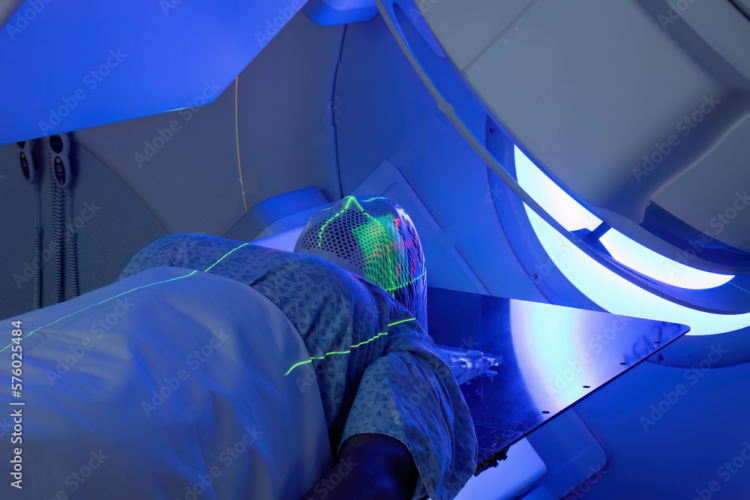
Treatment for HNCs is complex and can have life-changing consequences, such as mobility restrictions, pain, fatigue, psychological issues, and disorders affecting speech and people’s ability to swallow.3 6 Once treatment is completed, people with HNCs often require long-term follow-up support and rehabilitation. This can include access to dietetics, speech and language therapy, restorative dentistry, physiotherapy, occupational therapy, clinical nurse specialist (CNS) care, lymphedema services and clinical psychology services.3 Post-treatment effects for HNCs can be significant and unpredictable, and can cause distress and anxiety for people living with the disease.3
HNC care in the Thames Valley Cancer Alliance (TVCA) is issued via a centralised model that only provides care through Oxford University Hospitals NHS Foundation Trust.3 People in Swindon and Wiltshire are expected to travel to Oxford University Hospitals NHS Foundation Trust to receive care.2 Within TVCA, people living with HNCs have an average of 25 follow-up visits. People have cited long travel distances and high costs as major barriers to accessing follow-up care.3 This issue is exacerbated as HNCs disproportionately affect people who are the most socioeconomically deprived in the UK.
Solution
TVCA introduced ‘Care Closer to Home’ (CCH) in 2018, a pilot to redesign HNC follow-up care. The programme allowed residents in Swindon and Wiltshire to receive most of their follow-up and rehabilitative care closer to home at Great Western Hospital NHS Foundation Trust. The primary aim of CCH was to improve patient outcomes and experience of care for people living with HNCs. It also aimed to release capacity at Oxford University Hospitals NHS Foundation Trust, improve timely access to care for people with HNCs, and reduce delays in the diagnosis and treatment of HNC recurrence.3
CCH at Great Western Hospital NHS Foundation Trust provided individuals with HNC with a weekly multidisciplinary team (MDT) HNC clinic. The MDT was made up of healthcare professionals with a variety of specialties including maxillofacial, dietetics, speech and language therapy, and ear, nose and throat (ENT), as well as clinical nurse specialists.3 The MDT also had a patient pathway coordinator who is responsible for ensuring timely access to care for people with HNCs.7 CCH also provided individuals with HNC-specific rehabilitation education to facilitate self-care and the prevention of recurrence.3
What has been achieved?
An evaluation of the pilot showed that CCH had a significant benefit to people with HNCs. It reduced travel and waiting times, and reduced levels of fatigue and stress felt by individuals living with the disease. Lesser travel demands also decreased out-of-pocket costs for people with HNCs, and reduced the overall environmental burden.2
CCH was successful in improving capacity at Oxford University Hospitals NHS Foundation Trust due to HNC care being localised. The pilot also saw improved clinic attendance rates. Emergency room attendance in people with HNCs reduced from 31% to 23%, and emergency room admissions reduced from 69% to 46%.2 These changes resulted in operational financial savings and a more efficient use of resources. This improved efficiency also contributed to a reduction in cancer care backlogs by increasing the number of people that could be seen weekly.2
Since its inception, the CCH has expanded across the TVCA to increase the number of ENT and maxillofacial outpatient clinics to further reduce travel time and costs for people living with HNCs.3
Next steps
The evaluation of the CCH recommended that it be commissioned recurrently, and the care model should be rolled out across the TVCA. Amendments should be made to improve the delivery of patient education and to increase the uptake of holistic needs assessments by healthcare staff.3
References:
- International Agency for Research on Cancer. 2023. Estimated crude incidence rates in 2020, United Kingdom, both sexes, all ages (excl. NMSC). Available here: https://shorturl.at/bsxKP [accessed: December 2023]
- NHS South Central and West. 2021. Evaluating ‘Care Closer to Home’ pilot for head and neck cancer patients. Available here: https://www.scwcsu.nhs.uk/case-studies/evaluating-care-closer-to-home-pilot-for-head-and-neck-cancer-patients [accessed: December 2023]
- Thames Valley Cancer Alliance. 2021. Head and Neck Cancer Follow Up ‘Care Closer to Home’ Evaluation. Reading: South Central and West Commissioning Support Unit [accessed: December 2023]
- International Agency for Research on Cancer. 2023. Crude rate per 100 000, mortality, males and females: United Kingdom, Lip, oral cavity and pharynx - Larynx. Available here: https://shorturl.at/ruxIV [accessed: December 2023]
- Cancer Research UK. 2022. Head and neck cancers statistics. Available here: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers#heading-Zero [accessed: November 2023]
- National Institute for Clinical Excellence. 2004. Guidance on Cancer Services: Improving Outcomes in Head and Neck Cancers. London [accessed: December 2023]
- NHS Jobs. 2023. Patient Pathway Coordinator: Guy's and St Thomas' NHS Foundation Trust. Available here: https://www.jobs.nhs.uk/candidate/jobadvert/C9196-23-1965 [accessed: December 2023]