
Summary
Routine follow-up care for lung cancer patients often involves clinical assessments every 3–6 months. However, these standardised intervals may leave relapsing patients without medical input for weeks between appointments.1
Researchers in France developed a web-based algorithm to help oncologists take action at the first signs of a potential relapse.1 2 Lung cancer patients were asked to rate their symptoms every week using a short online form. The algorithm processed these symptom scores and automatically emailed oncologists if there were signs of a potential relapse. This algorithm, now built into a web and mobile application called Moovcare®, offers significant improvements in overall survival, relapse detection and healthcare costs for patients with lung cancer when compared to standard care.3-5
Challenge
Routine follow-up care for lung cancer patients commonly involves clinical assessments and imaging at standard intervals, often every 3–6 months. These non-personalised intervals may leave relapsing patients without medical input for weeks between appointments.1 In addition, repeated imaging is costly and may increase patients’ anxiety.2 At least 75% of lung cancer relapses are symptomatic, and these symptoms could be used to improve and personalise follow-up care.4 6
Solution
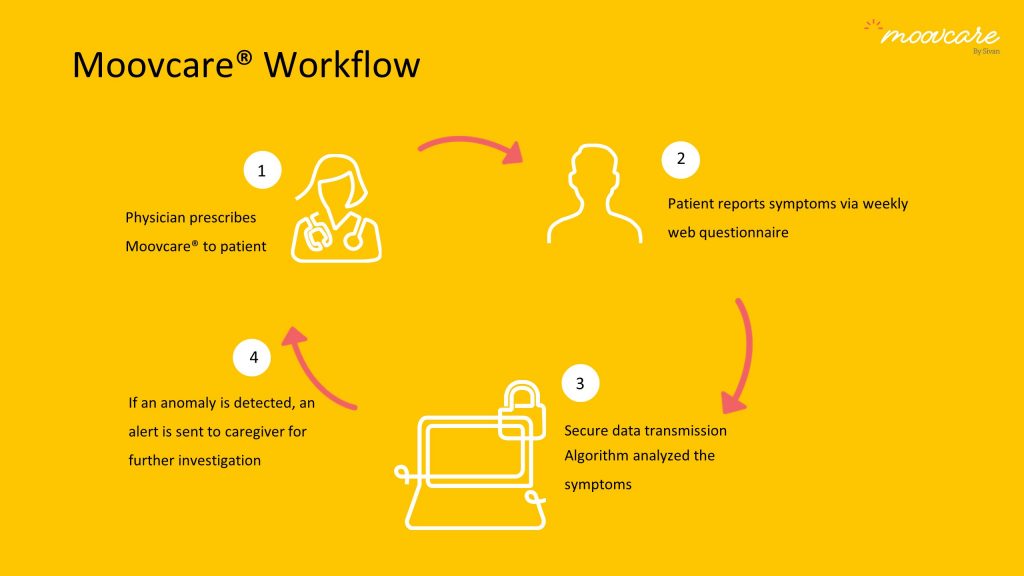
Researchers in France developed a web-based algorithm to detect potential lung cancer relapses based on patient reports.1 2 Lung cancer patients were asked to rate their symptoms (e.g. fatigue, pain or changes in weight) using a short online form every week. The algorithm processed these symptom scores and automatically emailed the patient’s oncologist when scores indicated a potential relapse. This process enabled oncologists to take immediate action (e.g. follow-up calls or imaging tests) at the first signs of a relapse.4
The algorithm was eventually built into a web application called Moovcare® in partnership with Sivan Innovation. Patients can submit weekly symptom reports through Moovcare® on a computer or mobile phone. Moovcare® is currently being used by 22 clinicians across 10 medical centres in France.
What has it achieved?
The phase III randomised clinical trial of Moovcare® was stopped early due to significant differences in median overall survival – 19 months in patients using Moovcare® versus 12 months in patients receiving standard care.4
From the interim analyses at 12 months:4
- Overall survival at 12 months: 78% of patients (Moovcare®) and 58% of patients (standard care)
- Imaging procedures decreased by 49% per patient per year, compared to standard care
- 86% of patients using Moovcare® had at least one alert leading to follow-up care from their oncologist
- 72% of first relapses were detected with Moovcare®, compared to 32% of first relapses in standard care
From the final analyses at 2 years:3
- Median overall survival was 22.5 months for patients using Moovcare®) and 14.9 months for those in standard care
From a study looking at the cost and cost-effectiveness of Moovcare®:5
- Imaging costs: €571 per patient for Moovcare® compared with €749 per patient with standard care
- Quality-adjusted life years (QALY) gained with Moovcare®: 4.6 years
Next steps
Following the effectiveness of Moovcare® for lung cancer patients in France, next steps include testing its application in other cancers and expanding to other European countries, Israel and the United States.
Further information
- The final results from the Moovcare® trial published in the Journal of the American Medical Association
- The abstract of the trial presented at the 2018 American Society of Clinical Oncology (ASCO) conference
- The Moovcare® website by Sivan Innovation
References:
- Denis F, Viger L, Charron A, et al. 2014. Detection of lung cancer relapse using self-reported symptoms transmitted via an Internet Web-application: pilot study of the sentinel follow-up. Support Care Cancer 22(6): 1467-73
- Denis F, Viger L, Charron A, et al. 2014. Detecting lung cancer relapse using self-evaluation forms weekly filled at home: the sentinel follow-up. Support Care Cancer 22(1): 79-85
- Denis F, Basch E, Septans AL, et al. 2019. Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA 321(3): 306-07
- Denis F, Lethrosne C, Pourel N, et al. 2017. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst 109(9): 1-8
- Lizee T, Basch E, Tremolieres P, et al. 2019. Cost-effectiveness of web-based patient-reported outcome surveillance in patients with lung cancer. J Thorac Oncol Available here: https://doi.org/10.1016/j.jtho.2019.02.005 [accessed: May 2019]
- Walsh GL, O'Connor M, Willis KM, et al. 1995. Is follow-up of lung cancer patients after resection medically indicated and cost-effective? Ann Thorac Surg 60(6): 1563-72