Summary
Radiation oncology (RO) is the treatment of cancers using targeted, high-energy radiation.1 RO is a fast-evolving field, but there are still consistent issues with incorrect dosages and their resulting toxicity, treatment delays due to a lack of workforce and infrastructure, and a lack of best-practice treatment guidelines.2 To combat these issues, the Michigan Radiation Oncology Quality Consortium (MROQC) was established in 2011.3 The goal of the consortium was to create a comprehensive clinical data registry of people receiving radiation treatment for breast, lung, prostate and bone cancers in order to facilitate treatment and dosage comparisons, as well as establishing best-practice guidelines for the delivery of radiation treatment.3 Since its inception, the consortium has grown to cover 27 radiation treatment facilities across Michigan.3 The consortium has led to the increased use of hypofractionation, reduced cardiac toxicity and the use of consistent nomenclature across these facilities. The consortium has also improved patient and healthcare provider experiences by increasing efficiency in treatment provision and data collection.2
Challenge
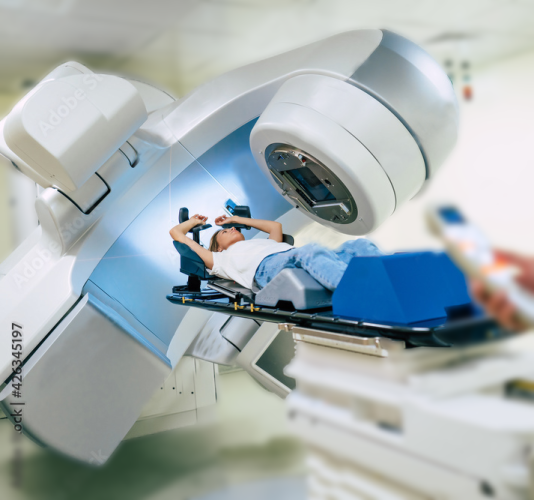
Radiation oncology (RO) is the treatment of cancers using targeted, high-energy radiation to shrink and even remove tumors.1 However, there are persistent issues in RO regarding toxicity due to suboptimal dosages, treatment delays due to a lack of workforce and infrastructure, inconsistent care guidelines, clinician adherence to treatment guidelines, and a lack of data on minimum effective dose.2 This lack of data means comparisons between treatments cannot be consistently made, and consistent best-practice themes are difficult to identify and enact.
These issues also negatively affect the patient experience, with 70% of RO patients from across the US saying they experienced a delay in receiving radiation treatment, and up to 45% of patients saying the side effects they experienced were much worse than expected.4
Disjointed care networks across the US means creating a cohesive set of best-practice guidelines for RO is difficult. Best-practice guidelines are guided by data, but these data are hard to collect and compare due to a lack of common nomenclature and unsystematic protocols for data collection.2
Solution
In 2011, The Michigan Radiation Oncology Quality Consortium (MROQC) was established with financial support from Blue Cross Blue Shield of Michigan and Blue Care Network. The consortium was set up with the goal to create a comprehensive clinical data registry of patients receiving radiation treatment for breast, lung, prostate and bone cancers. Data that are collected includes radiation treatment delivery and dosage, patient-reported outcomes and clinician assessments of treatment toxicity.3
The consortium’s overall objectives are to:3
- determine the best use of intensity modulated radiation therapy (a type of radiation oncology treatment that delivers highly targeted radiation beams to cancer sites) in lung and breast cancers5
- establish best-practice guidelines for the delivery of radiation treatment, with the aim of reducing radiation treatment times in order to reduce costs, as well as improving the quality, value and outcomes of treatment for patients
The consortium now consists of 27 radiation treatment facilities across Michigan, a coordinating centre that maintains the clinical data registry, and has over 300 members including oncologists, radiologists, medical physicians and nurses.2 3 To enhance quality improvement efforts, the consortium also has a working group for each cancer, consisting of ‘clinical champions’ (radiation oncologists who agree to implement best practices identified by the MROQC), doctors, medical physicists, dosimetrists, data scientists and administrators.3
What has been achieved?
Since the inception of the consortium, the application of hypofractionation – the administering of concurrent large radiation doses to reduce treatment time – has increased across the treatment facilities.6 This means that full treatment courses are delivered over a shorter period of time, thus saving money and improving the patient experience. The use of hypofractionation for bone metastases is estimated to have saved payers over $4.5 million between 2018 and 2020.2 Guideline-concordant hypofractionation for breast cancer has also increased from 47% to 97% of applicable cases.2
The systematic collection of the mean heart dose has helped to refine the minimum radiation dosage necessary. This helps to reduce over-exposure to radiation in people with breast cancer, thus decreasing cardiac toxicity and improving outcomes for patients.2 7
The consortium has also led to the use of mutually agreed-upon nomenclature. This is a factor that facilitates inter-institutional quality evaluations and the comparison of datasets.8 Standard nomenclature use by healthcare providers (HCPs) increased from 53% to 82% while treating people with lung cancer, and from 80% to 94% for people with breast cancer.9
As well as improving data-driven outcomes, the MROQC has also improved patient and HCP experiences by systematically surveying both groups as the consortium was implemented. It has enabled people living with cancer to be more involved in their own care, and allowed HCPs to improve their practice due to the culture of quality improvement and accountability.2
Next steps
The consortium continues to hone best-practice guidelines and improve patient experience by working to reduce mean heart dose during lung cancer treatment, and increasing the use of hypofractionation across cancers.9
The consortium has also set up an M-EQUAL working group that aims to identify and address health disparities experienced by people with cancer.10
References:
- National Cancer Institute (NCI). 2019. Radiation Therapy to Treat Cancer. Available from: Available here: https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy [accessed: May 2024]
- Jagsi R, Schipper M, Mietzel M, et al. 2022. The Michigan Radiation Oncology Quality Consortium: A Novel Initiative to Improve the Quality of Radiation Oncology Care. Int J Radiat Oncol Biol Phys 113(2): 257-65
- Michigan Radiation Oncology Quality Consortium. Our story. Available from: Available here: https://www.mroqc.org/our-story [accessed: May 2024]
- Shaverdian N, Yeboa DN, Gardner L, et al. 2019. Nationwide Survey of Patients' Perspectives Regarding Their Radiation and Multidisciplinary Cancer Treatment Experiences. J Oncol Pract 15(12): e1010-e17
- Cancer Research UK. 2023. Intensity modulated radiotherapy (IMRT). Available from: Available here: https://www.cancerresearchuk.org/about-cancer/treatment/radiotherapy/external/types/intensity-modulated-radiotherapy-imrt [accessed: May 2024]
- National Cancer Institute (NCI). hypofractionated radiation therapy. Available from: Available here: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/hypofractionated-radiation-therapy [accessed: May 2024]
- Pierce LJ, Feng M, Griffith KA, et al. 2017. Recent Time Trends and Predictors of Heart Dose From Breast Radiation Therapy in a Large Quality Consortium of Radiation Oncology Practices. International Journal of Radiation Oncology*Biology*Physics 99(5): 1154-61
- American Association of Physicists in Medicine. 2018. Standardizing Nomenclatures in Radiation Oncology. Virginia, US: American Association of Physicists in Medicine
- Dess RT, Sun Y, Muenz DG, et al. 2020. Cardiac Dose in Locally Advanced Lung Cancer: Results From a Statewide Consortium. Practical Radiation Oncology 10(1): e27-e36
- Michigan Radiation Oncology Quality Consortium. M-EQUAL. Available from: Available here: https://www.mroqc.org/m-equal [accessed: May 2024]