
By Amy Rosvold
Save Your Skin Foundation
How the research began
In November 2019, All.Can Canada hosted an inaugural multi-stakeholder roundtable meeting to share findings on top areas of inefficiency in Canadian cancer care from a pan-Canadian survey and find agreement on the priorities for All.Can Canada. Roundtable participants agreed that the priority area of focus should be ensuring swift, accurate and appropriately delivered diagnosis as the entry point into the cancer care system.
Understanding the current diagnosis experience of Canadian cancer patients
The first step was to conduct an environmental scan to understand the current state of the cancer diagnosis experience in Canada. Specifically, this included identifying outcomes that matter most to patients, reviewing promising practices in cancer diagnosis, and exploring areas of inefficiency in the cancer diagnosis process that represent opportunities for improvement. This research took place from June 2020 to March 2021and included a literature review, thirty qualitative interviews with cancer survivors, and a survey of healthcare providers across Canada.
Highlights of findings
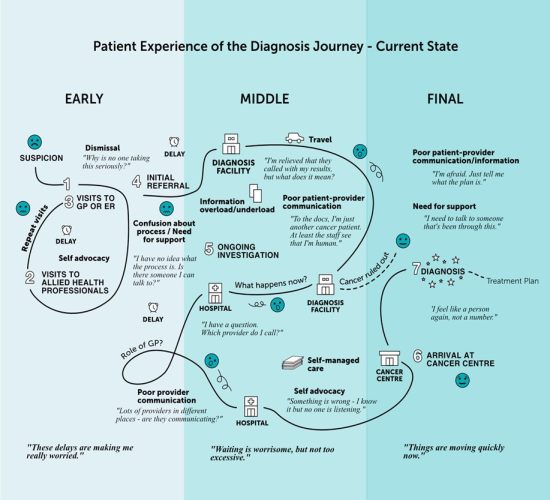
This figure is a snapshot of what our research found to be the current state of the diagnosis process for people in Canada.
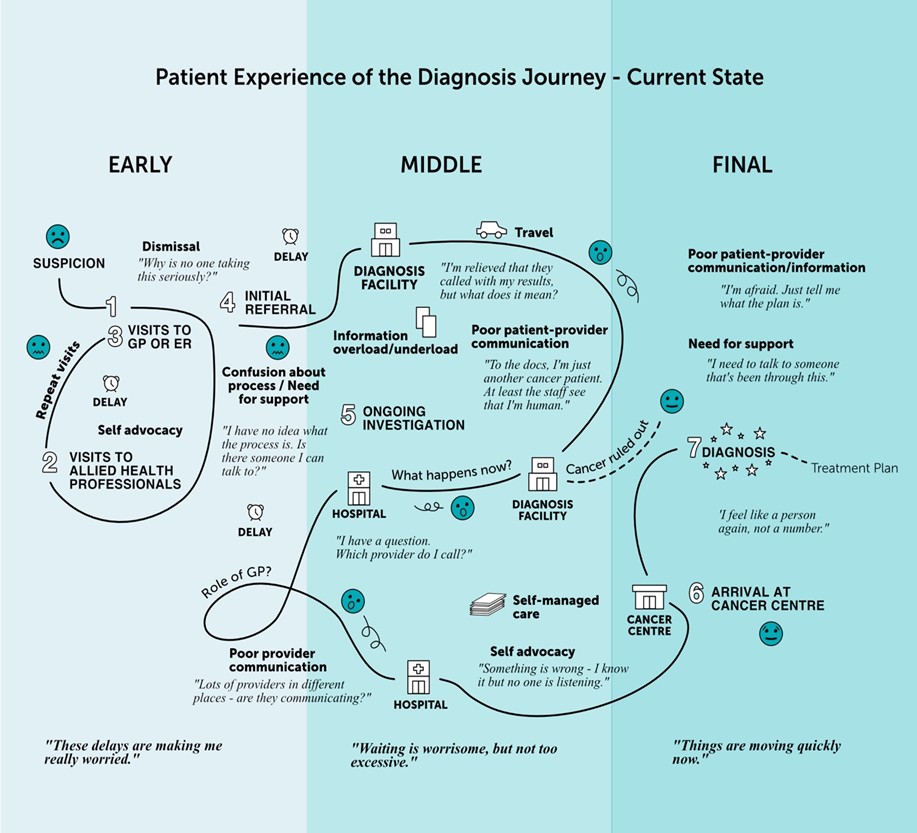
From the moment a person tries to interact with a healthcare provider over a suspicion of cancer to the point they receive their diagnosis, seven outcomes are critical.
1. Swiftness of the process
Eliminating unnecessary delays in the cancer diagnosis process will positively impact a person’s mental health and well-being and may improve health outcomes. Rapid referral pathways and optimized roles for laboratories and diagnostic centres, including telepathology, help achieve this.
“Getting results quickly may not have much impact in terms of survival but I think in terms of quality of life and the diagnosis experience it’s very important”.
– Female 67, breast cancer survivor
2. Concerns validated by primary care providers
Primary care providers need to take patient concerns seriously and initiate appropriate referrals. Supporting primary care providers with clinical decision supports, risk assessment tools, standardized care pathways, and provider education on cancer types, symptoms and pathways are opportunities for improvement.
“The biggest thing I’ve heard in all of this is you’re young, you’re fine. I was twenty-nine when I got diagnosed. If people keep brushing it off, we’re going to miss a ton of stuff. That age discrimination and the lack of awareness from the doctors…that could be the difference between saving someone’s life or not”.
– Female 30, melanoma survivor
3. Excellent patient-provider communication
Providers and patients need to communicate effectively throughout the process of symptom investigation so that patients stay informed, remain in control, and feel cared for. Fortunately, providers’ communications skills can continually be improved.
“The specialist just bustled in, said this looks like it could be cancer, you need to go for a biopsy, and then left. This was one of the most emotional moments in my life and I couldn’t even tell you what he looked like. The tech was like, can I get you some water? Can I hug you? It was like humanity when I needed it. I get they’re busy and time is tight but I just didn’t feel taken care of by the doctors; I felt taken care of by the staff”.
– Female 40, breast cancer survivor
4. Effective provider-provider communication
To ensure continuity of care in a discontinuous diagnosis system, healthcare providers, including primary care physicians and oncologists must communicate effectively with each other if they are to stay abreast of a patient’s diagnosis trajectory and make informed and timely decisions about their care. Technology is key to achieving this outcome.
“One person at this facility is telling you that you need a biopsy and someone else at this other facility is saying you don’t…how can this be urgent and necessary in one clinic but not in another?”
– Female 38, breast cancer survivor
5. Better information
Clear and accessible information is needed by patients throughout the diagnosis process. The type and amount of information varies by individual and by phase of the diagnosis journey.
“At that moment you don’t want to listen to a thirty-minute dissertation on what melanoma is. You just go holy crap, okay, what do we do about it?”.
– Male 64, melanoma cancer survivor
6. Integrated psychosocial support
To cope with the looming threat of a cancer diagnosis, psychosocial support must be available and integrated into patient care right from the start alongside diagnostic testing and medical procedures.
“It’s not just my breast that has cancer, it’s my body and my brain you know. So, you have to treat the whole body, you can’t just treat the affliction”.
– Female 40, breast cancer survivor
7. Integrated care
A dedicated care coordinator who is working as part of a multidisciplinary team to help navigate the diagnosis process would address inefficiencies and enhance patient experiences resulting in more timely and accurate diagnosis.
“The techs and nurses were wonderful. Very clear about what the test was for, what they were looking for. They called before every appointment to remind me, what to prepare in terms of meds. It meant the world to get these calls because I was prepared for every test”.
– Female 70, lung cancer survivor
What does the future look like?
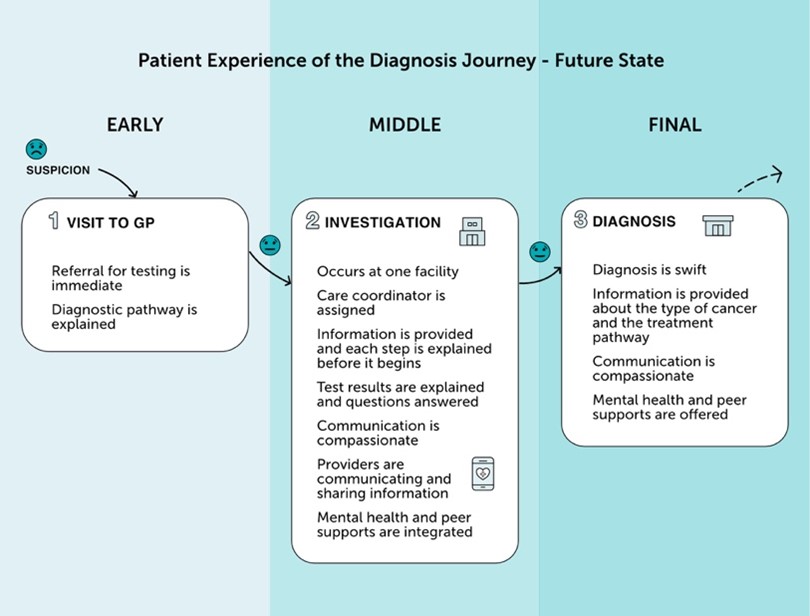
This research not only showed us the labyrinth most people currently experience when trying to diagnose a suspicion of cancer, but also provided a clear vision of what an improved, future state for cancer diagnosis in Canada could look like. The figure below offers a snapshot of what we envision the diagnosis journey should look like for people in Canada who are investigating a suspicion of cancer.
Conclusion
This environmental scan unveiled inefficiencies in cancer diagnosis in Canada but achieving an improved future state does not mean starting from scratch. Examined together, the findings are encouraging. There are numerous opportunities and good practices included in the full research report that, if adapted, spread and scaled for jurisdictional and regional needs, are an excellent place to begin the realization of a future, more desirable state of cancer diagnosis in which these seven outcomes are achieved for everyone. The full report will be published at the end of 2021.