
photos: © framez.

Overview
At the 20th anniversary of the European Health Forum Gastein, All.Can invited stakeholders to adopt a different perspective to tackle the question of how to make cancer care more efficient. Our workshop, entitled ‘Making cancer care more efficient – what role can different stakeholders play?’, asked participants to sit at tables representing different perspectives. The groups at each table then discussed how to improve efficiency in cancer care from that stakeholder group’s point of view.
First, we heard from Vivek Muthu of Marivek Ltd. (who also moderated the session) and Kathy Oliver, founding Co-Director and Chair, International Brain Tumour Alliance (IBTA).
Dr Muthu explained how ‘a euro or a dollar spent on ineffective healthcare is a euro or a dollar not spent on effective healthcare.’ He also highlighted that ‘patient outcomes are decided on the processes of healthcare – and we need to turn that on its head.’
Emerging themes from the literature review
Ms Oliver led us through the first findings of the literature review for the All.Can patient survey on waste and inefficiency in cancer care. This is the first survey of its kind and aims to identify, from the patient perspective, where efforts are most needed to improve the focus on patients and reduce waste in cancer care.
From the findings, patients see waste and inefficiency manifest themselves as:
- Delays and wasted time
- Poor communication and limited information
- A disconnect between patients’ needs and the care they receive
- A fragmentation of care, and a lack of follow-up.
We heard that a study of public perceptions on the benefits of breast and prostate cancer screening in nine European countries found that patients are not always aware of benefits and risks of interventions:
- 92% of women overestimated the benefits of mammography screening tests, or did not know the benefits
- 89% of men overestimated the benefits of PSA screening, or did not know the benefits.
Other illuminating findings included:
- A study in Norway, Holland, Italy and Canada found that 1 in 3 patients don’t receive pain medication appropriate to their pain level
- Over €7.2 billion could be saved in Germany every year through better coordination of care leading to reduced hospital admissions.
- A survey of oncologists in Italy found that a survivorship plan was only delivered to 9% of breast and colorectal cancer patients on discharge after treatment.
We also heard about the PROCHE programme and one manufacturer’s child friendly MRI scanners, both of which are described in the All.Can policy report.
Ms Oliver finished by pointing the way forward in tackling inefficiencies:
- More focus on patient experience and outcomes measures, rather than ‘traditional’ clinical outcomes
- Using real-world data to understand the impact of new interventions in practice
- Artificial intelligence to aid decision-making and personalise care solutions
- Data collected and used to drive a continuous cycle of improvement in patient care.
‘Waste is not just money,’ Ms Oliver emphasised, ‘but time, quality of life and missed opportunities for patients and their families.’

The workshop
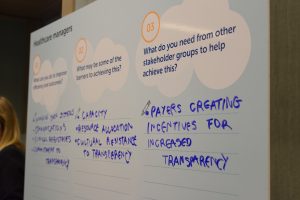
The audience was then split into eight stakeholder groups, each represented by a different hat: patients and caregivers; healthcare professionals; biomedical science industry; payers; academia and research; policymakers; non-biomedical industry; and healthcare managers. Following discussion at the tables, a representative of each table reported their ideas to the other groups.
Each table was presented with three questions for discussion. Some of the common ideas raised are as follows:
What can you do to improve efficiency and outcomes in cancer care?
- Integrated care models
- Better use of digital technology and data (with an emphasis on data protection)
- A focus on personalised, patient-centred treatment and care – with greater investment in palliative and end-of-life care.
What may be some of the barriers to achieving this?
- Lack of capacity, time, trust and data
- Complex regulation
- People working in siloes and the need to change organisational culture towards a patient-centred approach.
What do you need from other stakeholder groups to help achieve this?
- Earlier, more accurate and reliable information
- Increased transparency on outcomes of care
- Trust and willingness to listen, action ideas and cooperate between all stakeholders.
Panel discussion
To finish off the session, we had a panel discussion. The panel comprised Deepak Khanna, Senior Vice President and Regional President EMEAC, MSD Oncology, and four members of All.Can: Kathy Oliver; Birgit Beger, CEO, European CanCer Organisation (ECCO); Tit Albreht, Head of the Centre for Health Care, National Institute of Public Health, Slovenia; and Dr Wendy Yared, Director, Association of European Cancer Leagues.
Ms Beger called for clearer governance structures to be established to ensure patients can be an active part of policy discussions.
Dr Albreht agreed that patients need to be more involved in the implementation and evaluation of cancer care as they can ‘show us the reality of the healthcare system’. He observed that follow-up care was often incredibly unstructured and asked, ‘What is the environment a patient is returning to? What support do they need?’ He called for research to be focused and actionable, and said that we cannot assume a single outcome is valuable for all patients, but rather that there is a need for constant communication.
Mr Khanna noted the importance of building health literacy, and noted that ‘an educated patient can navigate through their healthcare system and use their resources’.
Ms Oliver warned against working in silos, and decried how people are sometimes not re-employed once diagnosed, or following treatment, due to stigma around their condition, particularly in the case of brain cancer: ‘What a waste of talent,’ she said.
Dr Muthu reasserted the need for commitment to transparency, even (or especially) when ‘we might find answers we don’t like’.
Dr Wendy Yared took a question from the floor about how to ensure patient advocate groups are taken more seriously, and not seen as simply the ‘emotional’ voice. Dr Yared explained that emotional stories can be very powerful, but must be made credible through data.
In conclusion
The workshop was a fantastic success, with the room completely filled and attendees showing a real enthusiasm and willingness to engage.
An encouraging observation was that the need to focus on what matters most to patients was the focus of all discussions. All stakeholder groups recognised the need to work together in a constructive manner.
The uniqueness of All.Can, and its ability to bring all sectors and stakeholders together, was widely talked about after the session. One attendee mentioned how important it was to have an ‘honest broker’ like All.Can to bring together stakeholders, with different agendas, to work towards a common goal – ultimately leading to better patient care.
Our session truly showed that this was possible.
The Young Gasteiners were also in attendance at the session and wrote a blog on the EHFG website: http://www.ehfg.org/blog/2017/10/04/making-cancer-care-more-efficient-what-role-can-different-stakeholders-play-f2/
You can watch the presentations on a webcast of the event here.

What’s next?
The workshop was not simply an intellectual exercise; All.Can will be taking the thoughts and recommendations provided and integrating them within our research and communications over the next 12 months.
All.Can will be conducting the first ever survey into waste and inefficiency from the patient and HCP perspective throughout 2018. The findings from the UK pilot will be released in March 2018. We are also working with ICHOM to investigate the meaning of ‘value’ in cancer care, how to quantify it and how to measure it, so that variations in care can be more effectively understood.
As was stated by Suzanne Wait (All.Can secretariat), ‘All.Can aims to become a hub for best practice and point the way to solutions, not just talk about problems.’
We are always looking to collaborate and form partnerships. If you are interested in finding out more about All.Can, please get in touch.
Together #WeAllCan.